In the complex field of addiction research and treatment, there are two constants that have shaped the course of the $400 billion addiction industry and the one million+ people it employs for more than seven decades. The first is the belief that a dysregulation, or impairment, of the brain’s mesolimbic dopamine system leads to substance abuse and other addictions. The second is the idea that addiction is a chronic disease or condition that cannot be overcome, but whose symptoms must be managed daily for life.
Meso-what? 
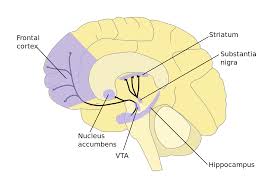
Reward Pathway
Very simply, there is a brain characteristic found common to people with addiction. It has to do with the regulating function of the brain system referred to as the reward pathway which is responsible for releasing and transmitting neurotransmitter dopamine from the more primitive midbrain, through the emotion-governing limbic region, to the executive frontal cortex region. It is perhaps the most influential area of the brain as it is the means by which we evaluate what is or is not rewarding to us.
In general, the head of the pathway responds to stimuli by releasing neurotransmitter dopamine in amounts proportional to the perceived intensity of each stimulus. The greater the stimulus, the greater volume of neurotransmitter released; the more neurotransmitter dopamine transmitted and received, the greater the feeling of reward or pleasure. No two people respond exactly the same to any given stimulus. For some, a walk in the park is a big deal, while for others it takes a roller coaster ride.

It is common for people with addiction to have reward systems that release and transmit relatively lower volumes of neurotransmitter dopamine than the average person in response to a control stimulus, such as a short video. They also are more likely to have fewer appropriate receptors standing ready to receive the released neurotransmitters, and to top it off, they probably have relatively higher neurotransmitter thresholds to reach before the actual transmission process can begin. The effect is that these people feel comparatively lower levels of reward or pleasure from that control stimulus than the average person. They are left wanting more.
Working from the long-held belief that addiction is caused by some structural or functional problem in the reward system, when the necessary technology became available, researchers seized on it, and set out to find the flaw. What they found instead, was this distinction in neurotransmitter volumes. And from that observation, though they could not objectively detect or quantify the point of difference, researchers concluded that people with this brain characteristic were led to use substances that were sufficiently stimulating to release the neurotransmitter volumes needed to successfully communicate a meaningful degree of reward or pleasure.
With continued technology advances, the reward system was found to extend to the brain’s frontal (executive) region, and researchers concluded that as sub stances were used repeatedly to deliver needed rewards, the behavior ultimately would bond with the persons’ executive brain region in their pre-frontal cortex. And there it would take on true meaning and importance as the only way for them to experience reward. Researchers marked closing bond as the transition to full-blown addiction[i].
stances were used repeatedly to deliver needed rewards, the behavior ultimately would bond with the persons’ executive brain region in their pre-frontal cortex. And there it would take on true meaning and importance as the only way for them to experience reward. Researchers marked closing bond as the transition to full-blown addiction[i].
Because even with treatment, people did not recover fully from addiction, but instead tended to relapse after periods of improvement, researchers further concluded that the brains’ closing bond with the substances (or other intense behaviors) was unbreakable, that the addiction was chronic, and that its symptoms must be managed daily for life.
Dysfunctioned and Chronically Addicted
For 80 years the industry has held steadfast to its beliefs and diagnosis of addiction as a chronic illness or disease stemming from an undetected brain system dysregulation (impairment) and brain changes brought on by subsequent substance use. Over the same period, the prescribed treatment remains lifelong symptom management defined as abstinence from the addicted behavior.
Firm in the belief that addiction cannot be overcome, treatment does not attempt to defeat the condition. Convinced that addiction cannot be defeated, research does not search for true solutions or ways to conquer addiction. Instead the full force of the $400+ billion industry and its million + person workforce is focused on improving processes for managing symptoms including the addition of medications, behavior training, and meditation.
overcome, treatment does not attempt to defeat the condition. Convinced that addiction cannot be defeated, research does not search for true solutions or ways to conquer addiction. Instead the full force of the $400+ billion industry and its million + person workforce is focused on improving processes for managing symptoms including the addition of medications, behavior training, and meditation.
Technology has been directed at finding and administering new pharmaceuticals, some utilizing recent knowledge in genetics, in an effort to stabilize moods, blunt cravings and deter substance use. Other advanced technologies have encouraged exploration of invasive techniques to manage symptoms including brain stimulation, surgical brain implants and more.
And though the technology is undeniably impressive, until there is an objective diagnosis, a detectable issue to address, a measurable (anything) to treat, or even a consistent means to measure and report treatment effectiveness, it’s no surprise that after spending trillions of dollars and dedicating the efforts of millions of experts to this one strategy of managing addiction symptoms, the industry has failed to slow the growth of addiction or to ease its wake of human and monetary devastation.
In spite of this poor performance history, the addiction industry is not veering from its two core beliefs. It is, however, exploring enhanced treatment methods, including direct and invasive means to manage addiction symptoms by altering the brain and the way it functions.
A New Urgency
It is this focus on changing the brain to change the symptoms that brings new urgency to our efforts to get the truth about addiction and its treatment out to those who need to know, now. Why the rush? Because we need to get out ahead of the issue. The two core beliefs propelling the addiction industry, the prevailing treatment method and this latest effort have never been proved or in any way objectively validated. In fact, recent research using advanced  imaging technology offers tangible evidence that both likely are false or at least seriously flawed[ii].
imaging technology offers tangible evidence that both likely are false or at least seriously flawed[ii].
It was one thing when these entrenched beliefs were the basis of a failed method to teach people how to live without substances or other addiction behaviors. But it’s quite another when the unproven ideas inspire scientists to pioneer genetically engineered pharmaceuticals, electrical brain implants or more invasive surgical procedures [iii]intended to alter peoples’ emotions, drives, impulses, decision making, and in general, how they pursue needed rewards or pleasure. These are the things that shape a persons’ individuality, that define their character and their personal identity. They should not be the target of another baseless and consequential method attempting to manage addiction symptoms.
quite another when the unproven ideas inspire scientists to pioneer genetically engineered pharmaceuticals, electrical brain implants or more invasive surgical procedures [iii]intended to alter peoples’ emotions, drives, impulses, decision making, and in general, how they pursue needed rewards or pleasure. These are the things that shape a persons’ individuality, that define their character and their personal identity. They should not be the target of another baseless and consequential method attempting to manage addiction symptoms.
That being said, I have to confess there’s a part of me that appreciates how clean and straightforward this direct approach sounds. On the surface, it’s seems so darned logical. Simply go in, make a few changes to a persons’ brain and, voila, instantly reduce or even remove the undesirable addiction behavior symptoms. I mean, why wouldn’t we?
But what if it were your brain or your child’s?
Knowing there’s no objective proof that something is wrong with your or your child’s brain to cause the harmful symptoms, but knowing for certain that the intended alterations would change part of what makes you or your child unique, would you authorize the treatment? Having no idea what effects the proposed brain adjustments might have on your or your child’s personal identity and character, beyond altering the unwanted symptoms in some manner, would you green-light the procedure? Of course not! Then why would you or anyone wish to proceed on this path with someone else’s child?
So What Do We Know?
1. There is no evidence to prove, or even to suggest, that the brain characteristic common to people with addiction leads them to use harmful substances or to engage in other harmful behaviors.
There is good evidence that this brain characteristic leads to a more driven personality and character; that it is common to highly motivated people across society.
And where would society be without such driven people? These are the people who will not be satisfied with the average, with doing just enough, but only will find satisfaction in going beyond and doing more?
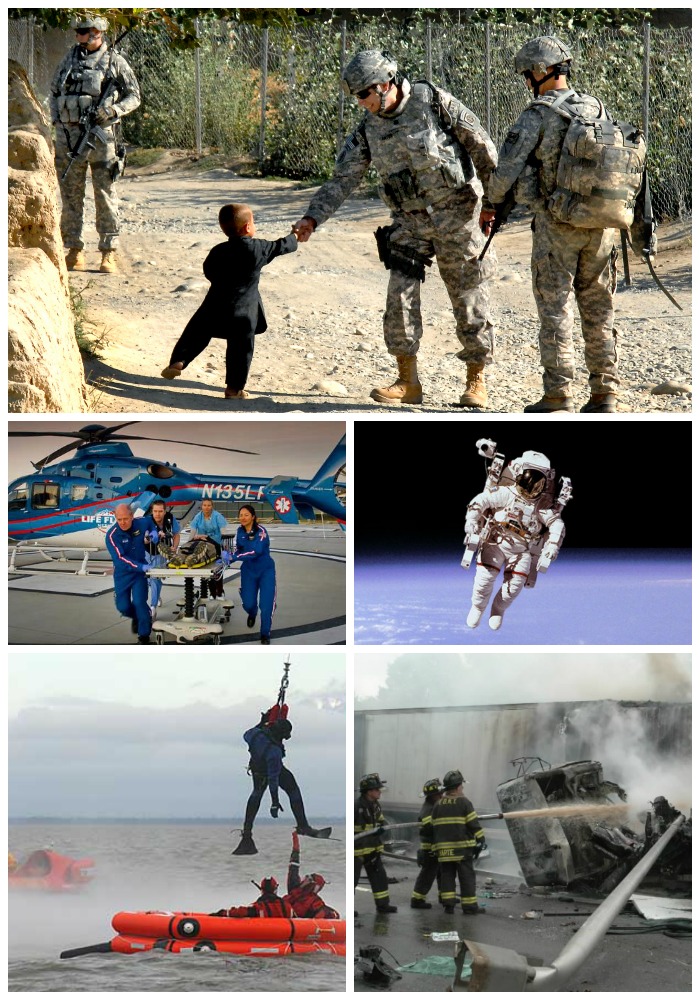 Where would we find our first responders, astronauts, explorers, entrepreneurs, race car drivers or our nation’s warriors?
Where would we find our first responders, astronauts, explorers, entrepreneurs, race car drivers or our nation’s warriors?
Would there have been a Steve Jobs, Ben Franklin, King David or disciples like Peter or Paul?
Yes, this brain characteristic is common to people with addiction, but valid research also demonstrates that it is common to CEO’s and other leaders.
The need for reward or sense of pleasure is basic to all people. And it leads all people to choose behaviors that satisfy their need. But the need is expressed differently in each and every person, as influenced by their brain and by their underlying character. It is not a matter of whether or not a person will meet their particular need. They will. It’s only a matter of how. It’s their choice.
While their uniquely functioning reward center influences the intensity and passion of the selected behavior, it’s their character – their faith, values, morals, beliefs, interests, likes, dislikes, tastes, preferences and personality – that guides the actual selection.
The often risky behavior of young people can be explained to a great extent by the fact that their character is still developing, as is the brain region that houses it – the prefrontal cortex, allowing the drives from their reward system to overwhelm any sense of better judgment that might tell them otherwise. (The fact that their prefrontal cortex is not fully formed until about 25 years of age, raises doubts about their ability to advance to full-blown addiction until then)
2. The evidence does not support the long-time chronic addiction diagnosis. It does suggest that addiction is a life-threatening, learned behavior pattern that can be fully overcome.
There is evidence that the closing bond of addiction is real and powerful and that brain changes can accompany substance abuse. But in the face of recent findings in neuroplasticity (brain changes), neurogenesis (new neuron growth), and even in the areas of brain self repair, it is unreasonable (bordering on absurd), to think that the addiction bond is unbreakable or that the related brain changes are lasting or have lasting impact.
There is evidence that harmful addiction behaviors are learned, that they are not the consequence of a fated brain function. People that require more intense stimuli to experience an adequate reward will be driven to more extreme behaviors. But nowhere is it even suggested that the behavior must be harmful or in any way is determined by a brain chemical setting.
There is evidence that telling people they cannot recover from addiction directly influences their behavior.
There is evidence that as people use substances they generally adopt part or all of the accompanying lifestyle. And as they do, they must alter critical elements of their basic character to accommodate it. The first change typically is to remove or distance themselves from God and all that comes with Him, as they cannot love God with His moral guidance and their addiction behavior the most. The next to go is family and the positive values that family generally stands for. When physical separation from family isn’t possible, the walls of emotional detachment can be equally effective to their need.
The new relationships and activities within their adopted addiction lifestyle bring about a change in their interests, likes, dislikes, tastes and preferences. And as the secrecy, darkness and volatile nature of the addiction culture become more present in their lives, their basic personality takes on the traits consistent with it. And finally, in due course, they will drop (or be dropped by) any remaining healthy friends, work, school and productive outside activities.
They have successfully realigned their very character with their new addiction lifestyle, creating a “fit” as compelling as the chemical bond of full-blown addiction. And both of these new bonds have taken place and reside in their brain’s prefrontal cortex, where they influence judgment, decision making and behavior.
But evidence demonstrates that even deeply bonded addiction character and behavior can be changed.
There is evidence that even deeply bonded harmful behaviors can be replaced by extremely productive, rewarding behaviors. And there is evidence suggesting that when the highly rewarding new behaviors, and the person’s faith, values and overall character are brought into alignment, until they fit comfortably, they can become “natural” and he or she can be freed fully from addiction’s bonds. (More about this later)
Time to act
Bottom line, we must alter or remove the two constants that have fixed the failed course of the addiction industry for decades, and now are leading it to unwarranted, consequential and even dangerous arenas. Before the industry is able to proceed further on this path, or along other avenues based on the long-entrenched beliefs, we must shine light on the fallacy of the two constants and on the premise they shape. We must expose invasive symptom management ideas, as well as other strategies to manipulate the brain as a means to manage addiction symptoms for what they are – desperate attempts to preserve an industry and its beliefs by sacrificing the individuality of those entrusted to their care.
We cannot confuse such thinking with similar propositions to manipulate the brain in an effort to manage Parkinson’s tremors, or introduce brain implants to aid patient recovery from stroke. The overall work being done in mapping the brain and building new technologies in neurobiology to advance treatment for serious illness and injury is important and needed. But to apply these remarkable advances in neuroscience to promote questionable or disproven premises risks doing harm to those treated, distracts from efforts to explore and validate new principles, and introduces questions of ethics.
Please join me in standing up for the truth about addiction. Trust that there is a better way. But know that it only will see the light of day when we stand together and demand it.
[i] Observation and reasoning shaped conclusions as the addiction itself cannot be objectively detected or diagnosed. [ii] See Brain Science, Like It’s Hard? [iii] http://www.technologyreview.com/news/527561/military-funds-brain-computer-interfaces-to-control-feelings/, http://www.geneticliteracyproject.org/2014/08/12/brain-breakthrough-genome-wide-association-studies-herald-advances-in-treating-mental-disorders/ http://www.thefix.com/content/probing-addiction-chinese-go-radical-brain, http://en.wikipedia.org/wiki/Psychosurgery