In the early days of my quest for a better way to treat addiction, one of the scientists helping me said the most valuable contribution I could make would be to come up with a definition of addiction that the different factions in the addiction industry could agree on.
I thought he was joking. But as time went on, I came to understand that he was dead-on. It seemed as though each “expert” resource had its own way of defining addiction – the field in which they were the acknowledged authorities. And though each definition began with the shared premise of addiction being a chronic condition, issues including the type of condition, where it was formed, what caused it, how it developed, how it was best diagnosed and how best to treat it, presented a range of viewpoints and painted very different pictures of a dangerous threat that showed no signs of abating.
 For the families and communities most closely affected, the lack of clarity or consistency from the expert community was confusing and added to their sense of helplessness when confronted with a diagnosis of chronic addiction.
For the families and communities most closely affected, the lack of clarity or consistency from the expert community was confusing and added to their sense of helplessness when confronted with a diagnosis of chronic addiction.
As I dug deeper though, it became clear that the challenge was far greater than just coming up with one set of acceptable of words to define “chronic addiction.” Rather, the real issue goes back to the fundamental understanding of addiction. Objectively, just what is it?
And right there was the big revelation! The problem wasn’t that there was widespread disagreement over the right way to explain what addiction is. Rather, it was that the disagreement stemmed from the simple fact that no one actually knows!
How we got here.
The story is well known. Seventy-five years ago, Bill W. and Dr. Bob set out to create a method for helping people who, like them, struggled with alcoholism or addiction, a condition they understood to be a chronic disease. The product of their work, Alcoholics Anonymous and the 12-Step Treatment Method, was introduced in 1939 and remains relatively unchanged today.
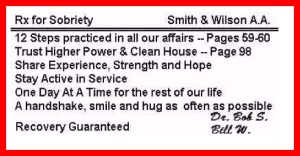
Their goal was to show others how to live as they did; for others to experience the advantages of living without alcohol. The men anchored their program on three core pillars: Faith in God; regenerated personal character; and new and healthy behaviors. And while the program can claim very limited effectiveness, the method has earned international recognition, drives a $400+ billion addiction industry, and is to be respected for its founders’ passion and compelling message that has built a community of driven people, desperate to break free of their addictions.
That said, no matter how well intentioned, deeply entrenched and widely accepted Alcoholics Anonymous and the 12-step treatment method might be, we can’t hide from the fact that while AA and its practices have grown steadily over the decades, the incidence and devastation of addiction have increased unhindered, and show no signs of slowing.
So what is wrong here?
Many critics will say the problem is in the treatment program – that the 12-steps need to be updated, upended or thrown out altogether. Others claim that the younger people entering treatment simply are not committed to the program – that until they are ready, nothing can help them. But in focusing on the details of the treatment itself, or waiting for participants to hit bottom, we overlook the real issue. Very simply, we are treating people for the wrong condition.
The 12-step program, used in over 90% of all treatment, is designed to treat a chronic and relapsing disease through daily management of symptoms. And while this focus was consistent with the evidence available in the 1930’s, findings from recent research suggest that addiction should be fully treatable, that full recovery can be achieved, and that full-blown addiction can be averted.
How Can It Be So Wrong?
The problem can be traced back to the fact that still today, even with all of our advanced science and high tech equipment, there is no way to objectively detect, diagnose, study, measure or monitor addiction. So in truth, no one fully knows just what, or precisely where, addiction is. There is no test to provide physicians and scientists with the objective evidence they need to point and say, “Here it is, this is what we’re dealing with!”
Until that time, researchers are forced to work with the information they have or can obtain through existing technology. And when they simply don’t have the capabilities to get at the information needed, they have a choice. They can stop their work and wait who knows how long, for technology to catch up, or they can apply their own reasoning to the accumulated information along with past assumptions, and build new assumptions to bridge the knowledge gap, allowing their work to carry on.
In other words, where the data path stops, scientists turn to faith, faith in themselves and their own reasoning powers, to form critical conclusions that lay the groundwork for further study and advances.
This is how the early scientists and physicians advising Bill W. and Dr. Bob arrived at their chronic addiction disease diagnosis. And it is this best-guess judgment that the founders of Alcoholics Anonymous made the cornerstone of their AA model and 12-steps treatment method. As the program gained a large following that included physicians, scientists, educators, and leaders of industry, the young addiction industry memorialized its principles and beliefs in what came to be known as the disease model of addiction.
 As this situation illustrates, the inherent risk of placing our faith in mans’ reasoning is mans’ great reluctance to let go of his own ideas, or the subsequent ideas that grow from them, even when confronted with objective evidence pointing a different direction. By the time brain imaging technology emerged in the 1980’s and 1990’s, offering the first real opportunity to objectively study the brain at work, the industry was firmly established in its decades-old beliefs.
As this situation illustrates, the inherent risk of placing our faith in mans’ reasoning is mans’ great reluctance to let go of his own ideas, or the subsequent ideas that grow from them, even when confronted with objective evidence pointing a different direction. By the time brain imaging technology emerged in the 1980’s and 1990’s, offering the first real opportunity to objectively study the brain at work, the industry was firmly established in its decades-old beliefs.
Was The Technology Ignored?
Researchers immediately embraced the new technology, but not to challenge or confirm their predecessors’ early bridge-building assumptions. Instead, when the emerging technology first allowed scientists to examine the functioning brains of addicted people vs. those of people without addiction, their research grew from the given that an abnormality or dysfunction in the brain’s neurobiology leads to substance abuse and chronic addiction. With that early idea now inarguably established within the industry, the task of research was to identify the malfunction.
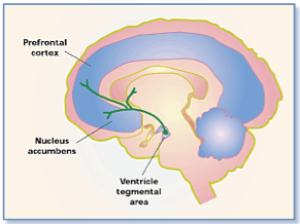
The brain’s mesolimbic dopamine system, or reward pathway, was seen as a likely point of origin for addiction. There, researchers identified a distinct functional characteristic shared among people with addiction: In response to control stimuli, their reward systems tended to release and transmit lower volumes of neurotransmitter dopamine compared with the reward systems of people that did not have addiction. The consequence of the lower NT volume was that people affected did not experience satisfying feelings of reward or pleasure, and were left craving more. Among addicted people with this reward system characteristic, the typical response was to satisfy their craving with intensely stimulating drugs and alcohol.
Researchers connected the dots and identified the characteristically lower NT dopamine volumes transmitted along the reward pathway of addicted people, to be a dysregulation of the mesolimbic dopamine reward system that leads to substance use and addiction. By positioning their findings in this manner, scientists categorized the brain characteristic and subsequent addiction, as a disease: An impairment to the normal function of a vital human system creating specific symptoms. And in doing so, they gave new credibility to the industry’s 8-decade old diagnosis.
However, because addiction still could not be objectively detected or diagnosed, and therefore could not be objectively studied, tested or treated, the matter of whether the disease was acute (meaning it was fully treatable and could be cured) or chronic (meaning it could not be fully treated or cured, but must be managed throughout the persons’ lifetime) was left unresolved.
Scientists once again put faith in their reasoning powers and concluded, that because no treatment method had proved to be effective at fully overcoming addiction symptoms, the disease must be chronic. (Never mind such pesky details as the treatment never attempted to overcome, but rather aimed at managing the symptoms.)
Does The Brain Function Actually Cause People To Use Drugs and Alcohol?
Studies among identical twins, who by definition have (near) identical brains and brain functions, report cases in which one twin would be a substance abuser and the other would not, and cite further examples where one twin had developed addiction while the other had not. These studies are good indicators that brain function alone is not responsible for driving people to use harmful substances, and that it certainly does not make them “genetically hardwired” for addiction.
Other studies using fMRI*[i] technology are revealing how certain types of brain function and brain anatomy influence, or at least correlate with, a person being inclined to sensation seeking, impulsivity activities or other forms of intensely stimulating behaviors. These studies do not suggest that the brain decided which specific behaviors or activities were pursued. Nor do the studies imply that the brain influenced whether harmful or productive behaviors satisfied the person’s craving for feelings of reward.
The research exploring the mesolimbic reward pathway, how it functions distinctly in every person, and how it can influence a person’s motivation, does not suggest that the brain region and function, in any way, direct or determine a particular type of behavior or course of action. The body of research does indicate that the brain region and function do influence the intensity drive that a person exhibits, but not the aim of that drive.
So when people certain people, by dint of their particular mesolimbic reward system, are identified as being vulnerable to addiction, it would be comparable to saying they are vulnerable to race car driving, to extreme athletics or to serving on God’s front lines in high-risk missionary work. To label anyone as specifically vulnerable (meaning helpless or defenseless) to addiction, not only is an imprecise application of research findings, but it also can be harmful to the person and to their motivation.
 And to define addiction as a brain system malfunction leading people to use and grow dependent on harmful substances is just wrong.
And to define addiction as a brain system malfunction leading people to use and grow dependent on harmful substances is just wrong.
But every day, educators, scientists, physicians, parents and others are depending on the industry’s expert definition of addiction to guide their thinking and actions on all matters related to addiction. And the standing definition, even in its various wordings, clearly communicates that addiction is a (genetic) dysregulation of the brain’s reward system that leads to substance abuse and chronic addiction.
How We Define Addiction Has Consequences
Yes, my science advisor was right. We must introduce a new definition of addiction. It must accurately reflect the most current research findings, make assertions that are thoroughly supported and use unambiguous language consistent with the scientific community while remaining appropriate to layman audiences.
How we define addiction has consequences and must reflect our concern for the wellbeing of the people we all are here to help, not for the reputations, careers and financial health of those people and organizations so deeply invested in the status quo.
I do question whether we will succeed in gaining industry-wide acceptance of a complete and unbiased definition for addiction. But I am confident that we can begin the process of replacing outdated assumptions with trustworthy information and understanding; of removing entrenched barriers, born of rigid and discredited beliefs, to open new channels for exploration and innovative ideas; of easing much confusion and fear surrounding addiction and of equipping people to recognize addiction and become part of the rebuilding effort.
[i] fMRI = functional magnetic resonance imaging technology that measures brain activity by monitoring changes in blood flow. Its value is in allowing us to “see” brain activity as it takes place, noting where and with what intensity it is occurring.